Why should I undergo endodontic treatment?
Pulp infection is a serious issue, and without addressing and treating the cause you may risk losing your tooth. As bacteria begin to multiply within the pulp, this can potentially lead to an abscess and other serious complications.
What caused this problem with my tooth?
Deep tooth decay is the most common cause of pulp damage. However, there are other factors that can expose your tooth's pulp to bacteria, causing pulp inflammation or infection. A traumatic injury (blow to the mouth), a cracked or loose filling, tooth fracture, repeated restorations and periodontal (gum) disease are just some examples.
What can my endodontist see or do that my dentist can’t?

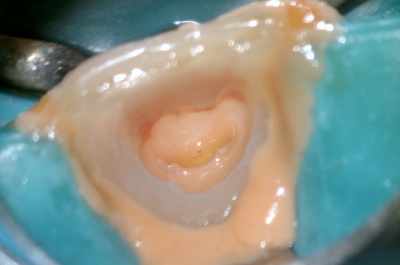
A photo taken under the microscope of a tooth that had root canal treatment elsewhere but did not settle post-treatment. After a few months the patient came in and we were able to diagnose a vertical root fracture (not visible on radiographs). It is very likely that had the patient seen an endodontist for the initial treatment, the fracture would have been diagnosed much earlier and saved the cost of the initial treatment.

A case where a lower molar had four canals present in the front root. These would have been impossible to locate without a microscope and likely would have led to a failed treatment.
A discoloured front tooth from behind with the canal accessed. Often the discolouration (and infection) extends in a thin sheet towards the tip of the tooth and is easily missed (and hence not cleaned out, with the infection and/or discolouration persisting).
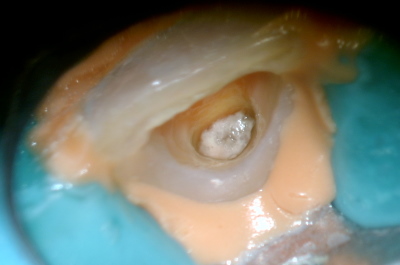
An almost fully calcified canal that requires very deep drilling to access and treat.

Another fracture line that is very fine and only visible under the microscope.
All these cases illustrate the value of having a root canal treatment done by an endodontic specialist.
What are the success rates of endodontic treatment?
Endodontic treatment at specialist level is often over 95% successful after a few years, depending on the study. However, the long-term success of treatment is subject to the condition of your tooth prior to receiving treatment, having proper restoration of the tooth and regular preventative care, and the way your teeth bite together. There is always a risk of tooth fracture (as there is with any tooth), but studies looking at dental implants versus endodontic treatment have shown almost identical success rates after 15-20 years.
How can I prepare for the actual treatment?
Ask your general dental practitioner or PN Endodontics any questions beforehand so you understand what treatment is being performed and how long it will take. You may be required to take medication prior to the procedure.
How do I take care of a tooth that has had endodontic treatment?
In the same manner you would with any other natural tooth. Maintain oral hygiene by flossing/brushing twice daily and avoiding a high sugar diet. Be sure to receive a bi-annual dental assessment, and crown back teeth that have had root canal treatment to help facilitate long-term survival.
Are there any alternatives to endodontic treatment?
Usually, the only alternative to endodontic treatment is extraction, although sometimes surgery is possible. The option after an extraction is to accept having a gap or fill the space with an artificial replacement such as a dental implant, removable denture or bridge restoration. Your endodontist will also discuss these options with you.
It should be noted that although no root-filled tooth has a lifetime guarantee, neither does any other treatment option, including implants. So keeping a tooth for as long as possible will effectively lengthen the lifespan of an implant or another treatment option.